How to Help Manage Idiopathic Pulmonary Fibrosis (IPF)
LEARN MORE
When it comes to managing IPF, taking action early is important. It can be hard, however, to know where to begin. On this page, we’ll help you take the first step by explaining how IPF affects your lungs, why early action is important, and what options you may have to help manage the disease.
Understanding the Impact of IPF Progression
Before deciding how best to manage IPF, it’s important to understand how it may affect your lungs. IPF causes progressive lung scarring, which means scarring of the lungs that gets worse over time. Sometimes this is called worsening fibrosis.
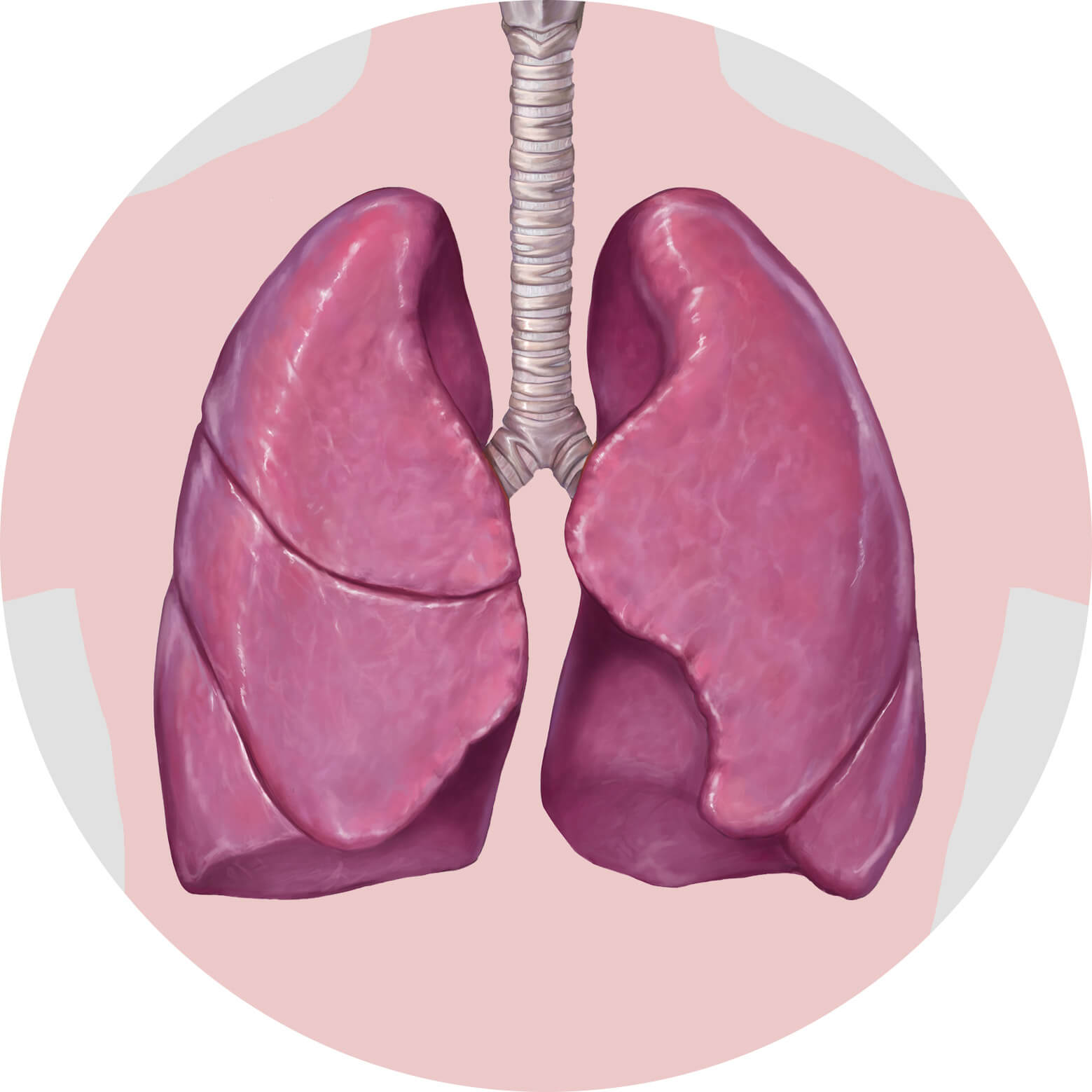
How does progressive lung scarring affect
the lungs?
Progressive lung scarring causes the lungs to become thick and stiff, making
it harder for oxygen to pass into the bloodstream. This damage is
irreversible and permanently affects the lungs’ ability to function
normally.

What does this mean for your day-to-day life and how you feel?
Breathing will become difficult, making even simple, everyday tasks, like walking or getting dressed, a challenge.
How can management options help?
There are management options available that may be able to help, including options that may help with IPF symptoms, options that may slow progression, and more.
Options for Helping to Manage IPF
Now that you’ve learned how IPF progression affects the lungs and why early action matters, it’s time to do something about it. Below is a list of options to help manage IPF. Talk with your healthcare provider about which options may be best for you.
Medication
While there is no cure for IPF, there are treatment options available that have been shown to slow IPF progression.
Pulmonary rehabilitation
Pulmonary rehabilitation is an education and exercise program designed to help improve overall well-being for people with lung conditions. Keep in mind that the purpose of pulmonary rehabilitation is to help with symptom management, but it does not help the underlying progression of IPF.
Oxygen therapy
Oxygen therapy uses an oxygen tank to deliver additional oxygen and help make breathing easier for those with low oxygen levels. Similar to pulmonary rehabilitation, oxygen therapy is designed to help manage IPF symptoms, but it does not help to slow the underlying disease.
Lung transplant
A lung transplant is an operation that replaces a person’s diseased lungs with lungs from a donor. Remember, lung transplants may be an option for some people with ILD, but not for everyone.
Palliative care
Palliative care is focused on managing symptoms and addressing the emotional, spiritual, physical, and social needs of those living with a serious illness like ILD.
Clinical trials
A clinical trial is a medical study that investigates how safe and effective a new therapy or technique is for managing a certain disease. Your healthcare provider can help you assess whether or not this is a good option for you.


You’re not alone in this
—Lungs&You® is just a phone
call away.
Do you have questions but no answers about your lung health? Are you looking to connect with someone who can help? Call us—we’re here for you.
Monday - Friday, 9 am - 6 pm ET
Keep in mind, Lungs&You® does not provide medical advice. Please consult with your healthcare provider if you have specific questions about your health.